What is Torticollis?
I’ve heard you talk about torticollis a lot, but can you explain what it is and why it is something to be concerned about?
Answer: Let’s start at the beginning & really break this down, because torticollis is very common and can be SO overwhelming, but is easily managed when addressed early!
What Is Torticollis?
Torticollis is tightening or restriction in expected range of motion of the sternocleidomastoid muscle (SCM) in the neck. Although often times, more than just this one muscle is involved and there can even be a bony alignment component for some, by definition the SCM is the ‘trouble spot’!
The image below shows the SCM muscle, one of the largest neck muscles, that has two origin points (the clavicle & sternum) and two attachment points (the mastoid process and occiput). It’s responsible for head & neck motions including; side bending to the SAME side as the muscle contracting (think, ear moving closer to shoulder while looking straight ahead), and rotating the head to the OPPOSITE side of the muscle contracting. These motions combined create a head position like the picture of my daughter above! There is often also a component of neck/head extension with torticollis, which gives the ‘chin tilted up’ position like in the above photo.
Simplified- when the RIGHT SCM muscle contracts, it brings your RIGHT ear towards your RIGHT shoulder, and turns your face towards the LEFT, often with a slight tilt upwards of your chin.
If you put your hand on the RIGHT side of your neck and do those motions, you’ll feel the SCM muscle bulge into your hands. And if you were “stuck” in this position, that would be considered a RIGHT torticollis.
So to recap, the PRIMARY (but not only) muscle responsible for torticollis causes a TILT in the SAME direction as the tight muscle & a ROTATION to the OPPOSITE.
Nice & confusing, amiright? 🤪🥴
Are There Different Kinds of Torticollis & When Does it Normally Occur?
Just to keep things extra confusing, yep…there sure are different kinds of torticollis! 🫣
While there are types of torticollis that primarily occur in adulthood including Spasmodic and Iatrogenic torticollis, this blog will only be covering the two common types of torticollis impacting children, including congenital torticollis (they are born with it) and acquired torticollis (it develops after birth).
1. Congenital Torticollis Common Characteristics:
Can be associated with other musculoskeletal concerns including hip dysplasia and plagiocephaly.
Plagiocephaly is one-sided flattening on the back of the skull with or without subsequent facial asymmetries (depending on severity).
When present, flattening on the skull and = facial asymmetries should be evaluated by a professional, as they can impact more than just ‘cosmetics’. If the forehead, ears, or jaw is shifted, things like vision, depth perception, body awareness & even speech & feeding can be impacted, depending on severity.
Most often caused by in utero positioning or trauma to the muscle during birth, but can also occur secondary to certain developmental or genetic conditions, or as a result of atypical development of the muscle and/or neck bones in utero
Occasionally results in a small lump within the muscle that can be felt when palpating
Typically responds very well to physical therapy interventions, especially when initiated as quickly as possible post birth
More common in first pregnancies, pregnancies with multiples, breech positioning, decreased amniotic fluid, and alongside hip dysplasia.
Torticollis is commonly associated with reflux due to the close connection between the SCM muscle and the vagus nerve, which is largely responsible for ‘rest and digest’ and can become excessively triggered when the SCM muscle is tight, as in torticollis. This overactivity of the vagus nerve in turn disrupts the digestion process and can result in reflux/GI symptoms. In fact, recent studies show a significantly higher rate of GERD in children with congenital muscular torticollis, when compared to the general population.
(2) Acquired Torticollis Common Characteristics:
Most often occurs in the first 6 months of life
While it can occur for non-serious reasons, acquired torticollis can sometimes be a sign of serious underlying health concerns that warrant further investigation as quickly as possible *especially if onset of the torticollis is associated with trauma, appears to be painful for the child, or is associated with onset of a fever.
Can occur in relation to benign paroxysmal torticollis (BPT), a condition characterized by episodes of head tilting which then resolve and can be accompanied with vomiting, dizziness, irritability/affect changes and/or fatigue.
How Do I Know If My Baby Has Torticollis?
Often times, the first signs of torticollis are a parent saying “my child loves to look one way”, or “my child always wants to turn to the....”, or noticing that your child’s head is always tilted to one side in pictures, etc.
In general, it is often subtle at first! If it’s not addressed, more significant signs can include asymmetries in the face, flattening of the back of the skull on one side (called plagiocephaly), neck & trunk tightness, limited range of motion or ability to track in one direction, only bringing one hand to their mouth, only rolling in one direction, or even curving of their trunk toward one side. It can also lead to scoliosis, feeding issues, contribute to reflux, potentially delay milestones, cause asymmetrical use of arms, and more.
More On Torticollis & Asymmetry
The video is a really quick example of what *can* happen with torticollis in regards to development of asymmetries in motor milestones.
Now - this is not always the case!!! There are times that torticollis is truly just a musculoskeletal issue that needs to be addressed, and it will resolve without the development of asymmetries or delays in milestones.
BUT, there are also times that asymmetries being present are one of the first things noted - things like parents seeing their child only looking in one direction, strongly preferring to use one hand, or roll in one direction, etc. These asymmetries can and often do impact the development of motor milestones, and absolutely need to be addressed in order to prevent further difficulty.
In the video above- you can imagine that if a baby is in the characteristic position of torticollis (head tilted in one direction and rotated to the opposite), that can lead to them looking only in one direction, seeing one hand much more than the other - which can lead to reaching more with that hand. If they are reaching and grabbing one foot more than the other, that can lead to happy baby to one side, ultimate rolling to one side from back to belly, and if on their belly the entire weight of their head is shifted off center, we can often see rolling from belly to back in only one direction as well!
Now … here’s the thing, please don’t panic. I want to share this information with you because torticollis is common, often goes unnoticed until it’s worse, and can impact many milestones, BUT in many cases, it can be managed with conservative treatment & the earlier the better for beginning treatment!
So What Do I Do If My Baby Shows Signs of Torticollis?
First, definitely speak to your pediatrician about what you’re noticing and discuss whether a PT evaluation is warranted! It is often ideal to have it assessed if torticollis is suspected - that will help determine the best course of treatment (whether at home stretches and positioning or actual skilled PT interventions), and ultimately help guide you to the best care for your little one!
Can Torticollis Come Back?
Unfortunately, torticollis can be tricky! The earlier treatment has begun, the faster results will be seen and typically, the duration of treatment required is shorter- in fact, 98% of infants with Congenital Muscular torticollis achieved normal range of motion within 1.5 months of PT intervention when intervention was begun BEFORE one month of age. 98%! That’s HUGE!
However, it is not at all uncommon to see ‘ebbs and flows’ in torticollis & related head positioning. When children are going through growth spurts, fighting an illness, working on a new milestone, even when they are just fatigued at the end of the day - you may see them drift back into that tilted head position. Typically, my recommendation is to resume your stretches & activities for a few days and DON’T PANIC! The vast majority of times, that positioning resolves again as they work through whatever is changing within their body - often times, in just a few shorts days.
However, due to this torticollis ‘trickiness’, in 2018, the APTA Academy of Pediatric Physical Therapy released Clinical Practice Guidelines (CPG), which contain evidence based recommendations on physical therapy management of Congenital Muscular Torticollis, including recommendations for discharge.
Those can be found HERE, however the most important information related to reoccurrence of torticollis & monitoring including the following criteria for therapists & parents/caregivers to consider:
Criteria for discontinuation of direct intervention:
Cervical rotation and lateral flex ion passive range of motion within 5 degrees of unaffected side (meaning when baby is relaxed and we move their head through turning and side bending, it should be nearly identical to the uninvolved side)
Symmetrical ACTIVE range of motion (meaning when baby is intentionally turning & side bending, the available motion is equal on both sides)
Age appropriate development
No visible head tilt
Parents clearly understand what to monitor as child grows
**Reassessment is recommended 3-12 months after discontinuing direct services OR when the child begins walking.
Want more info on torticollis?
Need More Milestone Support?
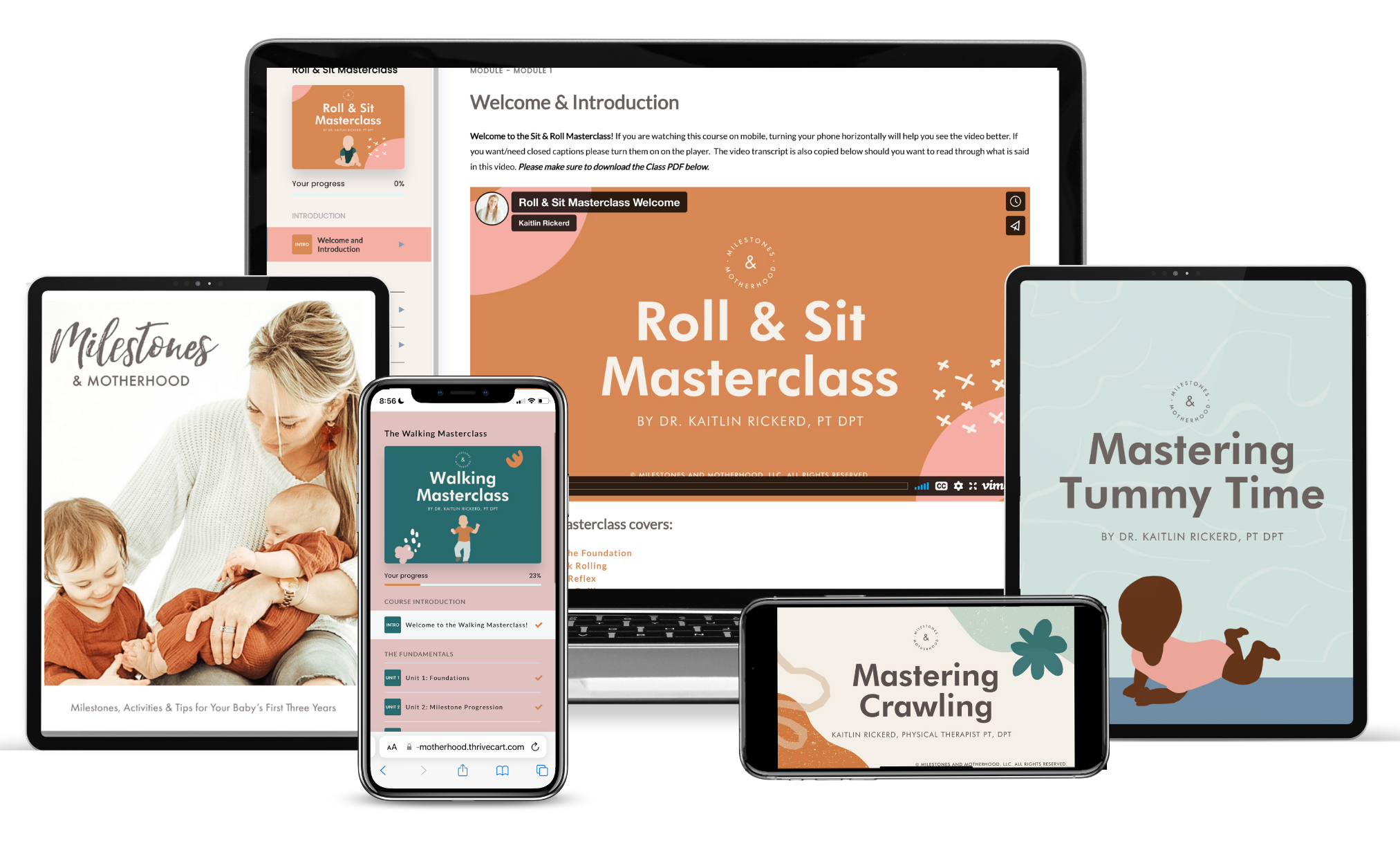
For developmental questions, tips and guidance related to milestones about tummy time, rolling & sitting, crawling and walking, check out KC’s developmental Masterclasses linked here.
KC is a pediatric doctor of physical therapy, wife and mom of three! She has spent her career working with children and young adults of all ability levels, and currently specializes in birth to three years.